On May 22, 2025, Department of Thoracic Surgery cooperates with Department of Gastroenterology to perform ICG-NIFR-guided precise dissection of the upper mediastinal lymph nodes in a minimally invasive radical resection of esophageal cancer.

A male patient, surnamed Zhang, was admitted to the First Affiliated Hospital (FAH) of Xi’an Jiaotong University (XJTU) for chest CT and gastroscopy biopsy and he was diagnosed with stage cT2N0M0 IB middle esophageal squamous cell carcinoma, with no local invasion or distant metastasis. Preoperatively, the teams of Professor Fu Junke from Department of Thoracic Surgery and Professor He Shuixiang from Department of Gastroenterology conducted repeated consultation and decided to adopt thoracoscopic and laparoscopic surgery with three-incision pattern (neck, chest and abdomen) combined with ICG-NIFR technology to achieve precise lymph node dissection. This technique had the following advantages. Preoperatively, ICG solution was injected surrounding the tumor through gastroscope. Intraoperatively, lymph nodes in the upper mediastinum were visualized by NIFR fluorescence imaging, which could accurately define the scope of dissection and avoid surgical complications such as injury of recurrent laryngeal nerve caused by blindly expanding the scope of dissection.
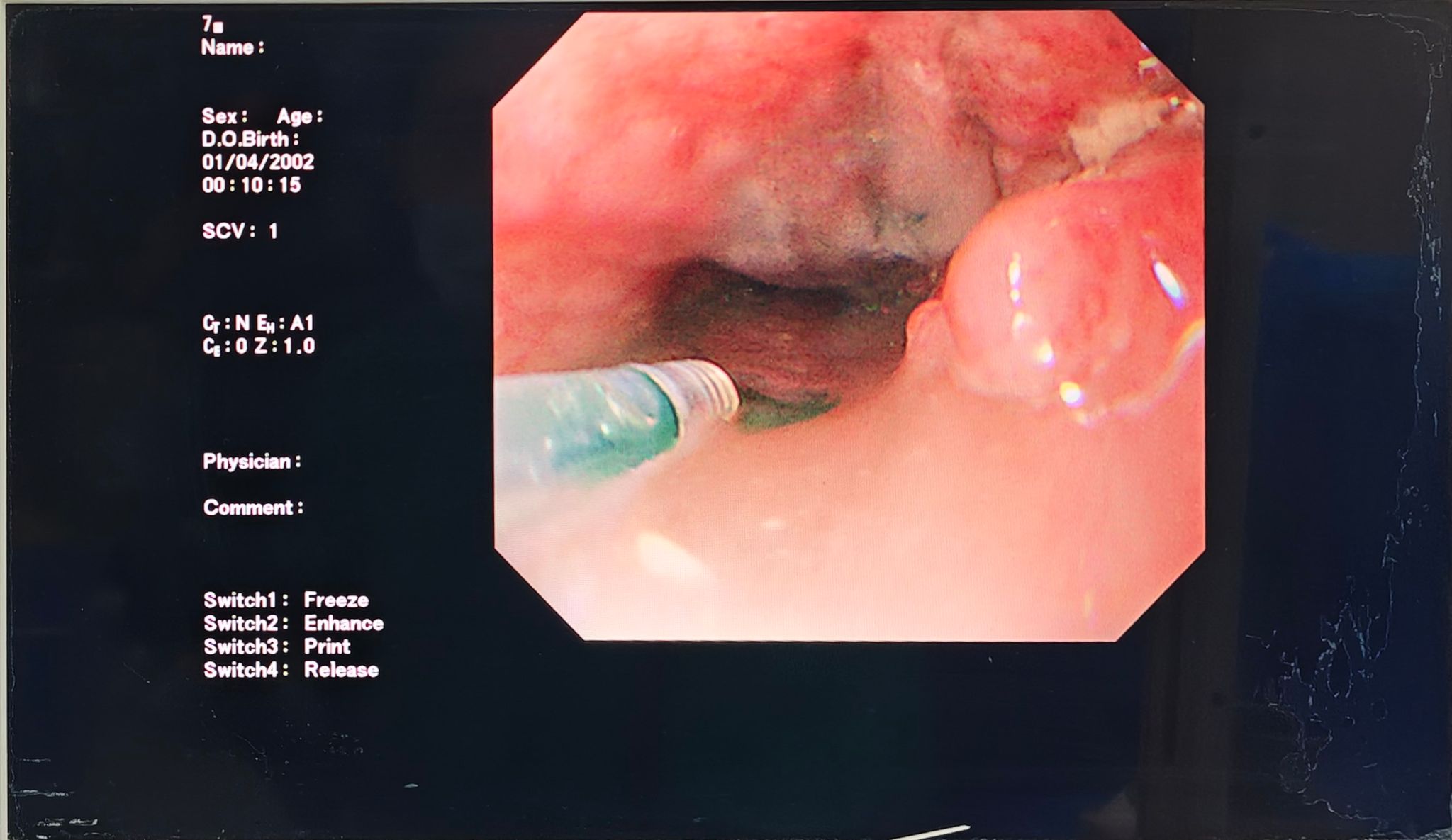
Intraoperatively, Professor Zhou Rongsheng from Department of Anesthesiology performed single-lumen tracheal intubation anesthesia. Physician Mi Chen from Department of Gastroenterology completed the injection of ICG solution surrounding the tumor under bedside gastroscope. Professor Fu Junke served as the chief surgeon, with the cooperation from Physician Jia Zhuoqi and Li Haijun. After thoracic esophagus was freed, it was switched to NIFR fluorescence mode, and the lymph nodes adjacent to the right recurrent laryngeal nerve, the carina and the upper mediastinum were explicitly visualized as the color of light green, and then EN-BLOC was performed. The undeveloped lymph nodes near the left recurrent laryngeal nerve and the main bronchus were not dissected. Intraoperatively, nerve protection was ensured, and gastroesophageal and cervical anastomosis was finally completed. At postoperative 4 d, the patient was recovered well.

Mediastinal lymph node dissection in radical resection of esophageal cancer plays a significant role in reducing recurrence or metastasis, whereas it is challenging to identify metastatic lymph nodes during operation. Applying ICG-NIFR in minimally invasive radical resection of esophageal cancer can achieve "visualized" dissection by fluorescence imaging, which not only ensures radical dissection, but also alleviates surgical trauma, shortens the length of hospital stay and reduces economic burden of patients. According to literature review, this is the first case of ICG-NIFR application in minimally invasive radical resection of esophageal cancer in northwest China, which has showcased remarkable clinical advantages.