On July 12, 2023, the team of Professor Yan Yang from Department of Cardiovascular Surgery of the First Affiliated Hospital (FAH) of Xi'an Jiaotong University (XJTU) successfully completed the first case of "suture-free valve implantation via minimally invasive intercostal incision for valve failure after Transcatheter Aortic Valve Implantation (TAVI)" in China for a patient with secondary infectious endocarditis only one year after interventional valve replacement surgery in other hospital. This innovative procedure brings a novel minimally invasive valve surgical regimen for more elderly and patients with severe valvular heart disease.

A 67-year-old male patient, surnamed Li, underwent TAVI 1 year ago due to severe calcified stenosis of aortic valve in a local hospital. He developed intermittent fever complicated with chest tightness and shortness of breath at postoperative 3 months. He was diagnosed with "infectious endocarditis, and aortic valve vegetation" in a local hospital. Considering only one year after TAVI and a history of hypertension and cerebral infarction, it is highly challenging and risky to perform open surgery again. Hence, the patient was admitted to Department of Cardiovascular Surgery of FAH for further treatment.
Echocardiography showed that moderate stenosis complicated with closure insufficiency and vegetation formation in the artificial aortic valve, 6 mm×4 mm in size, swinging back and forth along with cardiac cycle. After comprehensive consultation and evaluation of the patient's condition, Professor Yan Yang's team decided to perform a highly-demanding "suture-free valve implantation via minimally invasive intercostal incision for valve failure after TAVI", aiming to alleviate surgical trauma, shorten operation time and accelerate postoperative rehabilitation.
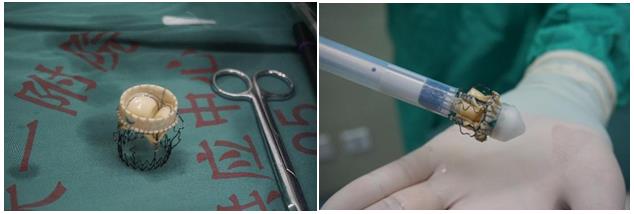
With intimate cooperation of Department of Anesthesiology and Perioperative Medicine, Department of Ultrasound Medicine department and other departments, Professor Yan Yang performed the surgery as the chief surgeon. After entering the thoracic cavity through the right second intercostal approach, TAVI valve was seriously adhered to the intima, and the entire stent was basically embedded in the intima of the aorta. It was highly challenging and risky to remove the artificial valve. Surprisingly, the surgical team completely removed the artificial valve and vegetation, measured the area of the valve ring, and selected No.25 suture-free biological valve with similar physiological status to maintain the patient's hemodynamics in the optimal state. It only took 10 minutes to implant, release and expand the biological valve. Postoperative esophageal ultrasound showed that the valve position was suitable, there was no perivalvular leakage, and the opening and mobility of the valve leaflet was normal. Although the whole procedure was highly difficult, satisfactory surgical efficacy was obtained. Postoperatively, the patient was transferred to ICU of Department of Cardiovascular Surgery for further rehabilitation.


Statistics demonstrate that perioperative mortality rate of the second surgery due to secondary infection after TAVI is as high as 40%-60% worldwide. Minimally invasive cardiac surgery combined with suture-free biological valve effectively mitigates surgical trauma, simplifies surgical procedures, shortens operation time, ensures surgical efficacy and maximizes the benefits of patients.