On the morning of November 6, 2022, a twin IVF pregnant woman at a gestational age of 35+6 weeks,surnamed Yang, suddenly showed fatigue, accompanied by vomiting. Vaginal fluid and amniotic membrane rupture occurred at 1 :00pm. Cranial CT scan confirmed a large area of cerebral hemorrhage.
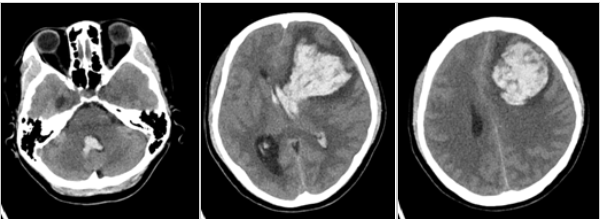
After the patient was transferred to our hospital, the possibility of cerebral vascular malformation was initially excluded. Relevant departments including Department of Obstetrics, Department of Neurosurgery and Department of Anesthesiology delivered multidisciplinary team (MDT) consultation. Preoperative evaluation and preparation were completed within just over 2 h after admission. She was scheduled to undergo emergency cesarean section and craniotomy for hematoma removal combined with decompressive craniectomy, which were jointly performed by obstetricians and neurosurgeons.
Approximately 30 min later, two fetuses with normal response and stable vital signs were delivered, and were transferred to Department of Neonatology for further treatment. After 4 h, Physician Xie Wanfu and Physician Bai Xiaobin from Department of Neurosurgery removed intracranial hematoma and performed decompressive craniectomy. Subsequently, the patient was transferred to intensive care unit (ICU) for further treatment.
After the operation, the patient remained in a slight coma state. Chief Physician Liu Yu and Attending Physician Zhang Lei from Department of Critical Care Medicine formulated a diagnosis and treatment regimen for this patient. Both non-invasive and invasive assessment was performed, and multi-modal neurological function monitoring was adopted to accurately assess the patient’s central nervous system function, circulatory capacity state, coagulation function and respiratory function. Medical staff explicitly introduced the treatment objective upon shifting. Physicians closely cooperated with nurses to achieve precise target management. Through concerted efforts of medical team from Department of Critical Care Medicine, the patient successfully weaned from the ventilator and received nasal cannula oxygenation within 3 days after admission to the department. She further received dehydration therapy, lowering intracranial pressure, anti-cerebral vasospasm, anti-convulsion, anti-epilepsy, nerve nurturing, brain protection and maintaining body temperature,etc. Cerebral hemorrhage and brain edema were alleviated. The patient became conscious and maintained stable blood pressure at 10 days after admission to the department. The lumbar cistern drainage tube was also successfully removed.
To accelerate the patient to restore normal life, early rehabilitation interventions, such as early-stage lung rehabilitation, passive activities of joints and muscles of limbs, were also actively started. Considering mental trauma caused by the disease and no visiting to ICU, the department regularly assisted the patient to have video chat with her family relatives, and played favorite news, TV series and music to the patient, which strengthened her confidence in postoperative rehabilitation.

Under around-the-clock attentive care from Department of Critical Care Medicine team and over 20-day postoperative recovery, the patient was successfully discharged and reunited with her two babies and family relatives.