Recently, the team from Department of General Surgery of the First Affiliated Hospital (FAH) of Xi’an Jiaotong University (XJTU) successfully performs total laparoscopic resection of a retroperitoneal tumor for a 9-year-old patient. Postoperative pathological findings confirmed the diagnosis of ganglioneuroma. The patient was properly recovered after surgery.
The child suffered from unexplained abdominal pain for 6 months, and the frequency of onset was gradually increased. Recently, the patient presented with vomiting and diarrhea, and was diagnosed with a huge "retroperitoneal tumor". Subsequently, the patient was transferred to Department General Surgery of FAH for further treatment. CT scan showed that the left retroperitoneal mass was located above the left kidney, below the pancreas and on the inferior side of the spleen. The left kidney, pancreas and spleen were all displaced by pressure. Branch blood vessels from the abdominal aorta passed through the mass, and the veins flowed into the left renal vein. The splenic artery, superior mesenteric artery and left renal vein all walked along the margin of the mass.
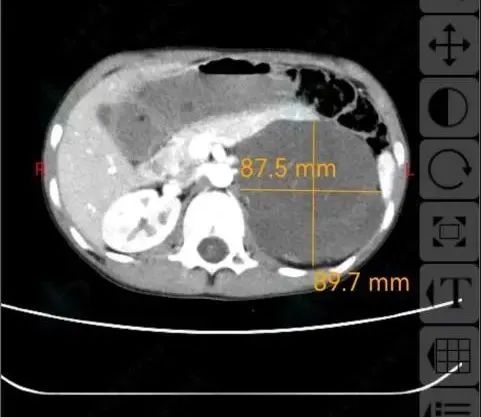
The retroperitoneal tumor expert team delivered preoperative MDT consultation, and determined a strict and feasible surgical plan for the patient. It is a highly demanding and risky procedure to achieve radical resection of the tumor without causing injury to other organs. On the day of surgery, Chief Physician Wang Shufeng performed laparoscopic resection of the left retroperitoneal giant tumor under general anesthesia. Laparoscopy showed that the mass was approximately 12×12×10 cm in size, located above the left kidney and below the pancreas, and closely adhered to the inferior vena cava, the lower margin of the pancreas, the left renal vein and the upper pole of the left kidney. The operation time was 3 h, and the surgical team completely resected the tumor under laparoscopy. Vital organs such as kidney, pancreas, spleen and colon were effectively protected. The tumor was resected via a merely 10 cm surgical incision. The surgical process was smooth, and vital signs of the patient were stable after surgery.
Because perioperative management of complex retroperitoneal tumors in children is highly demanding, postoperative 48-h intensive care and support plays a critical role in the success of surgery. Zhang Chun, Deputy Chief Physician from Department of Surgical ICU, made an individualized diagnosis and treatment plan for the child. Under comprehensive treatment of goal-oriented analgesia and sedation, refined fluid management, organ function protection, intimate monitoring of surgical complications and ERAS, tracheal intubation was removed at postoperative 1 h. The child had drinking water at postoperative 12 h, and could walk at 24 h after surgery. Meantime, Head Nurse Shen Cunyi led the nursing team to accelerate physical and mental recovery by playing music, reading books, toys and parental home companionship.

The patient’s physical condition was gradually improved and was transferred to general ward at postoperative 5 d. Postoperative pathological results confirmed the diagnosis of ganglioneuroma, a benign tumor of neural origin.
